Anesthesia Errors & Cerebral Palsy
While anesthesia plays an important role for many women in labor, an improperly-administered anesthesia (e.g., incorrect dosage) can lead to serious injuries to both the mother and child.
Epidural anesthesia is the most popular method of pain relief during labor. During this procedure, the anesthesiologist administers a drug or contrast agent in the epidural space of the mother’s spine. The process is usually safe, and in some instances, anesthesia can even cut short the amount of time a woman is in labor, making the childbirth process safer for both the mother and baby.
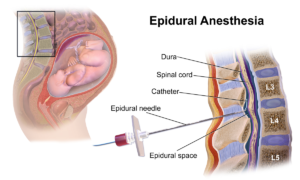
Epidural Anesthesia (credit)
Doctors, nurses, and anesthesiologists understand the dangers of adverse reactions all too well. As such, they are responsible for identifying any potential risks to the patient before administering any type of anesthetic. Failure to identify such risks could put the health of the mother and child at serious risk, and may constitute medical malpractice if the child suffered a serious injury (such as CP) as a result.
Risk 1: Fetal Distress
While doctors have been administering anesthesia for decades, risks associated with the practice still linger to this day. An anesthesiologist must act within an acceptable standard of care during the administration of an epidural, and they must make sure that the mother’s health checks out before doing so.
Any errors in this stage of labor can lead to a reduced oxygen supply to the child’s brain (hypoxia), which often results in permanent brain damage and/or the development of cerebral palsy.
Fetal distress signals should be closely monitored by medical staff following an epidural, and if detected, must be addressed immediately. Failure to do so will undoubtedly put the child at serious risk of suffering permanent brain damage.
Risk 2: Unusual Uterine Contractions
Anesthesia administration must be followed by close monitoring of the mother as well, in order to make sure there are no surprises down the line. For the most part, women who are given epidurals usually have protracted labor due to weak uterine muscle action. In these cases, doctors often administer Pitocin to stimulate uterine contractions.
Unfortunately if too much Pitocin is administered, contractions can be so strong and frequent that the uterine muscles compress the child’s head, which can also lead to brain damage. In other cases, abnormal contractions can prolong labor and leave the baby in the birth canal for too long, resulting in oxygen deprivation due to fetal asphyxia.
Risk 3: Low Blood Pressure
An epidural anesthesia will depress the central nervous system, which in turn may bring certain biological processes to a standstill. Low blood pressure is a very common side effect of an epidural, and it may cause the baby’s blood to pool in response to lack of sufficient pumping pressure from the mother. It is vital that doctors monitor the baby’s vitals using a fetal heart monitor in order to see how it responds to contractions, as well as monitor blood pressure.
It’s not uncommon for mothers on anesthesia to suffer respiratory arrest to the point of losing consciousness or being unable to breathe on their own. In some instances, IV cannulation or the accidental injection of the epidural solution into the bloodstream can happen, leading to seizures and convulsions that can have a direct effect on the mother and unborn baby.
Medication interactions can also occur if the mother has been given medication to soften the cervix to expedite labor. All these risks must be controlled by competent doctors in order to protect the unborn baby’s brain from injury. Failure to do so could open themselves up to a medical malpractice claim.
